This week, I had the pleasure of going on the GBMC Health Partners Lean Daily Management walk. I, along with members of my team, visited our Neurology Center, Ophthalmology, and Bariatric Surgery practices. I was so excited to see the incredible level of engagement of the staff in each practice. They are doing phenomenal improvement work to move us faster towards our vision!
In the Neurology Center, Kristen Stamathis, the Senior Practice Manager, presented a least waste metric. The team was working to better understand the causes of patients not coming for their appointment and how to reduce this “no-show” rate. Dr. Michael Sellman, the Medical Director, and Kristen know that the time neurologists spend with their patients is an incredibly valuable resource. With the aging of the population, there is an ever-increasing need for neurology consultations and there are very few neurologists in our community.
Literature suggests that the patient no-show rate goes up exponentially for appointments made more than 18 days before the date of their visit. People are more likely to forget about the appointment or have their needs met in some other way the more distant the scheduling date is from the appointment date. I pointed out that many restaurants will not allow you to make a reservation more than 30 days in advance because of this fact.
So, what should the team do to make sure appointments are not wasted? I told the group that my dentist texts me the day before the appointment and asks me to respond “Y” for yes if I can keep my appointment or “N” for no if I can’t. If I reply “no” or don’t reply at all, they give my appointment to another patient. For many restaurants that use OpenTable, I now get a prompt the day before asking me to confirm my reservation. We also discussed the commercial airline system where they calculate the average no-show rate and overbook the seats. They know that sometimes everyone will show up and then they must pay some passengers to fly later (Kristen and Dr. Sellman didn’t like the idea of paying some patients to come back another day…okay, I was only kidding) but by doing this, the airlines ensure that they won’t take off with empty seats from no-shows.
Of course, no reminder system is foolproof, but I was very proud of the team for the rigor of their study of the problem and their willingness to test new ideas.
A huge “Thank You” to our Elder Medical Care team!!!
Last week, our Elder Medical Care (EMC) Home Services Team provided Thanksgiving dinner to families in need. Last year, we helped 10 families enjoy their Thanksgiving Day holiday, but this year, the need was greater than ever, and our program rose to the occasion.
Thanks to the efforts of our EMC Home Services Team and the Notre Dame University of Maryland pharmacy students, 15 turkeys and more than $400 in cash and gift cards helped to provide a very nice Thanksgiving Day meal to two small assisted living facilities (ALF) -- the donation to Agape ALF was made in honor of Kathy Ruane -- and 15 families. The Thanksgiving dinners consisted of turkeys or rotisserie chickens, side dishes, bread, and dessert. Some of our families, who are not able to cook due to safety concerns, received ready to eat or microwavable meals. Providing families with a Thanksgiving meal who would otherwise not have had one is an all-hands-on-deck effort lead by the providers of the EMC Home Services Team.
A big thank you to Laurie Whelden, Yolanda Greene, Jessica Trizna, Asma Hussaini, and Dr. Freedman for helping with the deliveries, to Thelma Winn for picking up our donations from the Assistance Center of Towson Churches, Kathy Roberts for delivering frozen and fresh poultry around Baltimore County, and to the EMC/Advanced Care Management employees who donated their frozen turkeys and canned goods/money. We could not have done this without all of you and I am truly thankful for your kindness and generosity!
Friday, November 30, 2018
Tuesday, November 20, 2018
Thankful for You!
This Thursday is Thanksgiving Day. I would like to wish a Happy Thanksgiving to my GBMC colleagues.
Thanksgiving is a time to reflect on all that we have. I am very fortunate to have a wonderful wife and children, and wonderful friends and family members.
The GBMC family has a lot to be thankful for as well. We have a beautiful campus, great doctors, nurses, allied health professionals, and support staff working in the hospital, at GBMC Health Partners, and at Gilchrist. We are so lucky to have our fabulous volunteer auxiliary and tremendous community support. Members of the community serve on our GBMC HealthCare Board, the Philanthropy Committee, and the Gilchrist Board. Our governance bodies are made up of individuals who are dedicated to the mission of GBMC – a mission of health, healing, and hope for our community.
I am grateful for everyone who helps us care for our patients and I am grateful for the patients themselves, who entrust their care to us.
I also want to extend a special “thank you!” to all who will work on Thanksgiving, or who are working during the extended holiday weekend.
Again, wishing you all a joyful Thanksgiving!
P.S. What are you thankful for during this time? I’d love to hear about it – please leave me a comment!
Friday, November 16, 2018
We Earned An "A"
Last week, we got a report card of sorts and I am happy to report that we received an “A” grade! We achieved this high mark in The Leapfrog Group’s Hospital Safety Grades for fall 2018, which rates how well hospitals protect patients from errors, injuries, and infections. The survey assessed more than 2,500 hospitals across the nation, including 40 in Maryland. GBMC was one of only five hospitals in the Baltimore region and one of eight in the state to get an “A”! To see the grades, click here.
The Leapfrog Group, which launched its first hospital survey in 2001, began when a group of business leaders wanted to accelerate the improvement of hospital safety and worked with the Business Roundtable to review the evidence. If you would like to learn more about the survey, click here. The hospitals were given a letter grade from “A” through “F” based on several factors, including medical errors, accidents, injuries, and infections. The goal of the rankings is to determine a patient's risk of further injury or infection if they visit a particular hospital.
We should all be proud of this accomplishment. It is a measure of how well we are doing on our first Aim: the best health outcomes. We cannot be delivering the care we want for our own loved ones if patients are not safe from harm under our care. This “A” grade is another piece of evidence showing that we are moving towards our vision. We still have work to do but we have made great strides towards zero harm! I want to thank our entire team for all that you have done to move us to this point. I also want to thank Laura Hines, RN, SCNR, Director of Clinical Quality Outcomes and Carolyn Candiello, our Vice President for Quality and Patient Safety for their tremendous work in culling the data for the survey. Great work!
We are so fortunate to have Gilchrist in our system of care!
November is National Hospice and Palliative Care Month and I think It’s an appropriate time to recognize the Gilchrist team, led by Cathy Hamel and Dr. Tony Riley, who have designed an exceptional system of elder care and pediatric end-of-life care. Gilchrist has outstanding programs to keep elders well and to serve them as they develop illness and progress through to end of life. Our geriatricians assess patients in consultation, serve as medical directors in over 30 extended care facilities, manage the Gilchrist Rehabilitation Unit at GBMC, work with advanced practitioners to deliver in-home primary care, handle symptom management and palliative care for patients with terminal disease, and of course, they work with the fabulous Gilchrist nurses to deliver end-of-life care through Gilchrist Hospice. The work continues with families after the death of their loved one with bereavement support and counseling.
Recently, Gilchrist launched a new Integrative Medicine program that’s available to patients receiving treatment at our Sandra & Malcolm Berman Cancer Institute. Leading the initiative is the program director, Delia Chiaramonte, MD. In the program, cancer patients receive evidence-based interventions to alleviate the symptoms and the stress of cancer to improve their quality of life. Integrative treatment planning covers symptoms such as sleep problems, anxiety, depression, pain, nausea, and fatigue. Thank you, Gilchrist and welcome, Dr. Chiaramonte!
Last month, I had the pleasure of attending Gilchrist’s Taste of Howard County. This year’s theme was Merriment in Masquerade and the event featured food from more than 20 of Howard County’s premier caterers and restaurateurs. It also included more than one hundred bid items as well as a cash raffle. Over $200,000 was raised and all proceeds from the event will support Gilchrist Center Howard County, the only inpatient hospice in the county.
Over the last 24 years, Gilchrist has done so much to help so many people. We are so grateful for all that the Gilchrist team does every day.
Don’t Forget to Get Your Flu Shot!!
Currently, approximately 82% of GBMC employees and staff have gotten their flu shot. Our next FLU VACCINE EVENT is this Friday, Nov. 16, in the ED concourse, from 7AM - 7PM; or, you can receive your vaccine in Employee Health any Mon-Fri, from 7AM - 4PM. Thank you for getting your immunization.
Celebrating Nurse Practitioner Week
Please join me in celebrating GBMC’s outstanding Nurse Practitioners (NPs) this week. Across our nation, there are more than 220,000 NPs who provide care to millions of Americans. We have excellent Nurse Practitioners working in our hospital, in our physician practices, and in Gilchrist. They help us reach our vision of a patient-centered system of care every day. Please join me in thanking them this week!
Baltimore Magazine Excellence in Nursing
It's that time again - Baltimore magazine is collecting nominations for its Excellence in Nursing issue. Please vote for the colleagues you most respect! The survey, which ends on November 30, may be found here.
Thanking Our Veterans on Veterans Day and Every Day
On Sunday, we commemorated Veterans Day and took the time to remember and pay tribute to the brave men and women of the U.S. armed forces who have served in the past and those who are serving today. My sincere gratitude to all members of the U.S. armed forces and their families who make sacrifices to preserve our freedom.
Friday, November 9, 2018
A GBMC Giant is Retiring
 This week, we began celebrating the outstanding career of Bennett J. (Ben) Beres. Ben joined GBMC HealthCare in February 2012 as Chief Operating Officer for Greater Baltimore Medical Associates (GBMA). He has made a huge difference in the functioning of our physician company in the almost seven years that he has been with us.
This week, we began celebrating the outstanding career of Bennett J. (Ben) Beres. Ben joined GBMC HealthCare in February 2012 as Chief Operating Officer for Greater Baltimore Medical Associates (GBMA). He has made a huge difference in the functioning of our physician company in the almost seven years that he has been with us.Ben and I previously worked together at Boston Medical Center. So, when we were looking for a new operational leader for GBMA in late 2011, I called him. I remember being ecstatic when Ben agreed to interview for the position.
I called Ben because I knew that he was a phenomenal physician practice manager and leader. He always started from the perspective of the patient, but he also looked out for those providing the care. It was important to him that physician leaders worked in partnership with practice managers. Ben was just the right person to oversee the implementation of our patient-centered medical homes. He completely embraced our vision of becoming an accountable system of care that the patient would experience as a whole. He championed extended office hours to include evenings and weekends and he led our work for better office throughput. Ben sent Sarah Whiteford, MD, and Ben Hand, MD, to the Virginia Mason Institute in Seattle to learn office flow science. They returned to work with our architects to design our Family Care Associates office in the Kahlert Pavilion. A hallmark of this office is that there is no patient waiting room. Patients go from the greeter station directly to the exam room.
Ben first partnered with GBMA Medical Director Dr. Mark Lamos and then with Dr. Harold Tucker, with whom he constructed the rebranding and relaunching as GBMC Health Partners. Ben has also done excellent work with our specialty practices.
In addition to being an incredible manager and leader, Ben is also an incredible human being. He is dedicated, hard-working, and always focused on making things better. Perhaps Ben will be best remembered for being the consummate friend. I have never seen anyone make as many friends and make them so easily as Ben. I believe that this occurs because he treats everyone with respect.
Ben has lived apart from his dear wife, Ellen, as she has continued her career as an internist at Dartmouth. They have each spent a lot of time traveling between Manchester, New Hampshire, and BWI and we, the GBMC family, have benefited from their sacrifices.
GBMC has been so fortunate to have Ben as a friend and colleague, as have I. We will miss him dearly, but we wish him the best in his well-earned retirement!
We will never forget Ben or his dedication to patients and his work at empowering physicians to lead. Therefore, we have decided to name the library at Family Care Associates, the Ben Beres Library. Please join me in thanking Ben for all that he has done for GBMC and our patients.
Thanking our Medical Staff Services Team
Each year, during the first week of November, we recognize the important role that our medical services professionals play in our healthcare system. During National Medical Staff Services Awareness Week, we thank all our staff who work behind the scenes to ensure our providers are properly credentialed, licensed, and trained in their respective specialties. Often called the “gatekeepers of patient safety,” the work our exceptional medical staff professionals do contributes to our system’s high safety and quality standards. We thank you for your efforts and dedication this week, and every week of the year.
I’d also like to celebrate the NICU’s recent recognition from the Maryland Patient Safety Council (MPSC), which awarded the GBMC NICU with a banner of excellence in the care of infants with Neonatal Abstinence Syndrome. This accomplishment is the culmination of two years of implementing best practices and compassionate care to our most vulnerable patients. As you can imagine, caring for newborns experiencing drug withdrawal because of in-utero exposure requires ongoing diligence and expert care. It’s an emotional and often difficult job seeing these infants through withdrawal while also helping to educate and support the mothers and families. I am extremely proud of the work being accomplished by our neonatal team.
 Finally, GBMC will be kicking off the season of giving by participating in #GivingTuesday. Giving Tuesday is celebrated each year on the Tuesday following Thanksgiving (this year it’s November 27th) and will benefit GBMC’s Child Life Program. Supporting our #GivingTuesday campaign means you’ll help provide toys, games, and other tools our Child Life specialists use to help ease the stress our pediatric patients often experience during their hospital stay. There are two ways to give this season – through the CrowdRise page and by gifting a donation through the Amazon Wish List. It’s amazing to watch our Child Life specialists help our young patients cope with the anxiety brought on by hospitalization, and I know they will appreciate the support.
Finally, GBMC will be kicking off the season of giving by participating in #GivingTuesday. Giving Tuesday is celebrated each year on the Tuesday following Thanksgiving (this year it’s November 27th) and will benefit GBMC’s Child Life Program. Supporting our #GivingTuesday campaign means you’ll help provide toys, games, and other tools our Child Life specialists use to help ease the stress our pediatric patients often experience during their hospital stay. There are two ways to give this season – through the CrowdRise page and by gifting a donation through the Amazon Wish List. It’s amazing to watch our Child Life specialists help our young patients cope with the anxiety brought on by hospitalization, and I know they will appreciate the support.
Friday, November 2, 2018
Working Smarter, Not Harder
Our hospital is a very complex system. What happens in one area of the hospital can have a major effect in what happens in another unit or department. Because of this complexity, it is difficult to maximize our efficiency such that no one is waiting to move to the appropriate place.
I have written in this blog before that we are students of flow. We are designing our systems and matching the demand for services with the supply of caregivers throughout our organization. When we design our systems, hold ourselves accountable to the design, and match capacity to demand, our patients move one at a time in beautiful choreography. This is called single patient flow. On the other hand, when we have no design or don’t follow our designs and rely on hard work alone, we frequently have patients stuck in a bottleneck.
Humans can overcome bottlenecks by working around them or exerting more pressure or influence to get through them. This is known as expediting. An example of expediting is when we take someone away from their usual work to complete a task that the people who normally do it cannot accomplish. An example would be having a housekeeping manager race to clean a room because many dirty rooms have been called in for cleaning at once in the early evening. Rather than fixing the root cause of the problem, in this case the batching of discharges, we send someone to work around the problem in the moment to get the patients what they need. We have improved patient flow, but we will need to fix it again the next day because the batching of discharges has not been fixed. Smart leaders will learn the cause of the bottleneck, redesign the system, and not become complacent with the short-term success of expediting.
We know about the Hawthorne Effect as well, that when a problem gets focused on, it usually gets better without anyone redesigning anything. This is generally because the people involved, knowing that their work is being studied, work harder and faster to overcome the poorly designed process. This is the reason why we are so focused on getting the work redesigned first before we celebrate what looks like an improvement. If the gains are due only to shining the light on the problem, we lose the gains as soon as the light is turned off.
Our flow team and our Emergency Department leaders have been spending time studying and redesigning our processes to move admitted patients out of the Emergency Department to an inpatient bed as soon as possible after the decision to admit has been made. This system is very complex, and it has many sub-systems. The ED physician must enter the admitting order, a bed must be identified as empty on the appropriate unit, and then it must be cleaned. The ED nurse must communicate with the receiving nurse, as does the ED physician with the receiving physician. Transport must be notified and arrive to move the patient.
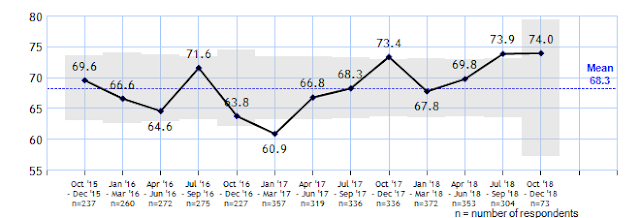
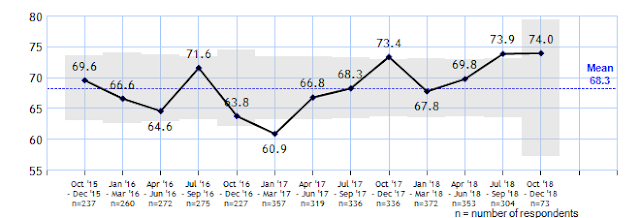
The number of patients waiting in the Emergency Department to be moved to an inpatient bed at 7 p.m. is a metric on the Executive Lean Daily Management Board. Every morning, we review this metric to learn the reasons that patients are waiting. Much progress has been made through system redesign and I am so proud of all involved. And while we still have processes in need of further improvement, we are working smarter rather than harder. Take a look below at the results of their hard work.
Patient Engagement Question — Wait Time in ED Before Admitted (Quarterly)
I have written in this blog before that we are students of flow. We are designing our systems and matching the demand for services with the supply of caregivers throughout our organization. When we design our systems, hold ourselves accountable to the design, and match capacity to demand, our patients move one at a time in beautiful choreography. This is called single patient flow. On the other hand, when we have no design or don’t follow our designs and rely on hard work alone, we frequently have patients stuck in a bottleneck.
Humans can overcome bottlenecks by working around them or exerting more pressure or influence to get through them. This is known as expediting. An example of expediting is when we take someone away from their usual work to complete a task that the people who normally do it cannot accomplish. An example would be having a housekeeping manager race to clean a room because many dirty rooms have been called in for cleaning at once in the early evening. Rather than fixing the root cause of the problem, in this case the batching of discharges, we send someone to work around the problem in the moment to get the patients what they need. We have improved patient flow, but we will need to fix it again the next day because the batching of discharges has not been fixed. Smart leaders will learn the cause of the bottleneck, redesign the system, and not become complacent with the short-term success of expediting.
We know about the Hawthorne Effect as well, that when a problem gets focused on, it usually gets better without anyone redesigning anything. This is generally because the people involved, knowing that their work is being studied, work harder and faster to overcome the poorly designed process. This is the reason why we are so focused on getting the work redesigned first before we celebrate what looks like an improvement. If the gains are due only to shining the light on the problem, we lose the gains as soon as the light is turned off.
Our flow team and our Emergency Department leaders have been spending time studying and redesigning our processes to move admitted patients out of the Emergency Department to an inpatient bed as soon as possible after the decision to admit has been made. This system is very complex, and it has many sub-systems. The ED physician must enter the admitting order, a bed must be identified as empty on the appropriate unit, and then it must be cleaned. The ED nurse must communicate with the receiving nurse, as does the ED physician with the receiving physician. Transport must be notified and arrive to move the patient.
The number of patients waiting in the Emergency Department to be moved to an inpatient bed at 7 p.m. is a metric on the Executive Lean Daily Management Board. Every morning, we review this metric to learn the reasons that patients are waiting. Much progress has been made through system redesign and I am so proud of all involved. And while we still have processes in need of further improvement, we are working smarter rather than harder. Take a look below at the results of their hard work.
Patient Engagement Question — Wait Time in ED Before Admitted (Quarterly)
Subscribe to:
Posts (Atom)









