Friday, February 1, 2013
Standardizing The Work Of Rounding
Humans do things in batches to make the most efficient use of their time. Years ago before I paid my bills on-line, I would put them in a pile on my desk at home and then write the checks all at once towards the end of the month rather than getting the checkbook out every day when each bill came in. This made sense if my goal was the efficient use of my time. However, “batching” is a huge problem in large complex systems because the “downstream” process is often idle, waiting for the batch to be run.
“Batching” is a big problem in healthcare. (See: “Getting Better at Getting Better” and “Using Technology and Standardized Work to Make Care Easier and More Reliable”) I remember when I was a practicing pediatrician and was caring for inner city children with high environmental exposures to lead. I would see a child on a Wednesday and have to wait a week for the blood lead level because the test was only done on Tuesdays. Occasionally, we would find out that a child had very high levels of lead 7 days after I should have admitted him to the hospital for treatment for acute lead toxicity. The tests were all done on one day because it made sense for the lab….but it didn’t make sense for the system that was trying to take care of the children. The system would have been better served by the tests being done one at a time as they were needed by the physician to make the decision to help the patient.
At GBMC, we too have problems created by batching. One that we have committed to fix in this fiscal year is the problem of admitted patients in the Emergency Department waiting to go to an inpatient bed. The rate of arrivals of patients to the ED starts picking up around 8 in the morning. By late morning, there are a significant number of patients who have been identified for admission at GBMC as in most hospitals in our country. But in almost every hospital in our country, few admissions actually leave the ED until late in the afternoon or early evening. Why do they wait? Well, there are a number of reasons but the most common is that they are waiting for a discharged patient to leave a bed in order for the bed to be made ready for the next patient. Why are the patients not leaving sooner? Well, again there are a number of reasons, but the single biggest reason is that the doctors, nurses, and other clinicians have not yet done the work of discharge.
Late last year, we did a value stream analysis of the work required to discharge a patient and physician rounding was identified as a significant opportunity for improvement. The long wait time for a patient waiting to go home is nothing more than a characteristic of the system that we have designed to discharge them. Our doctors and nurses are working very, very, hard. It is not about them, it is about the system.
If you were waiting to drive your mother home from the hospital and you were told early in the morning that she was ready to go but that it was going to take until the late afternoon before the team could do the work required to discharge her, you would not be happy. We owe it to our patients and their families to redesign our systems when they are not meeting our needs. Our vision is “to every patient every time we will provide that care that we would want for our own loved ones.” And, we don’t want our patients waiting unnecessarily.
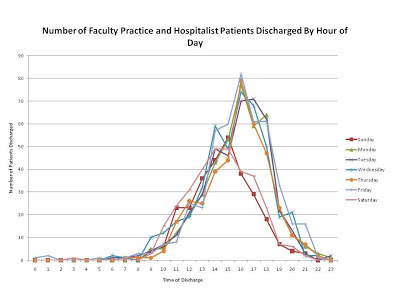
I’m excited to report that last week we did a weeklong Kaizen event (a review by staff to reduce waste and improve efficiency) on physician rounding. A team spent a week studying physician work on the medicine hospitalist service and the medicine resident service and they mapped all of the daily work and then started testing changes to that workflow. Team members were Jeff Biedronski, Michael Finegan, Lisa Griffee, Stephanie Mayoryk, Dr. Fred Chan, Dr. Ezza Khan, Dr. Rekha Motagi, Dr. Eugene Obah, Dr. Sajeet Sohi, Kathy Bull, Keith Jackson, Deb McCaffrey, Cate O'Connor, George Bayless, and Dr. John Saunders. The Team began with the evidence- the data on when physicians write the discharge order (peaking at 2 PM) and when patients actually leave (peaking at around 4 PM).
Their work included trying to plan the evening before who would be ready to leave the following morning; improving the signout from physicians going home in the morning to those coming in; and planning discharges to do a few each hour rather than all at once.
This work is very exciting because it “smoothes” or “load levels” the amount of work across the daylight hours, so if a patient is ready to go home early in the morning, they can, rather than have everyone go home in the afternoon. This effort is another example of GBMC learning to utilize engineering concepts as we standardize our work toward our goals. It’s not about relying on hard work and good intentions alone, nor about telling doctors and nurses to work harder and faster. I am so excited to show you the same graphs as above on the second day after the team implemented some changes!
Our goal is not for everyone to go home in the morning, rather the goal is for everyone to home as soon as possible after they no longer need to be in the hospital. We look forward to making this goal a reality in 2013.
Welcome to the GBMC Family
We have some very exciting news to share! We recently received commitments from two local outstanding physicians to join the GBMC Medical Staff. Drs. Michael Sellman and James Bernheimer will join the Department of Medicine as employed members of GBMA and will be leading our Division of Neurology and nationally-accredited Stroke program beginning July 1. This is an exciting and important event for GBMC as we build a strong hospital-based neurology practice.
Go Ravens!
One final thought for the week – Go Ravens! The GBMC family wishes the best of luck to our Baltimore Ravens in this weekend’s Super Bowl XLVII. Hopefully many staff, patients and visitors have enjoyed the lights, banners and other “Purple Fever” activities throughout the GBMC HealthCare system this week and I look forward to celebrating a victory for the Ravens on Sunday night!
5 comments:
Thank you for taking time to read "A Healthy Dialogue" and for commenting on the blog. Comments are an important part of the public dialogue and help facilitate conversation. All comments are reviewed before posting to ensure posts are not off-topic, do not violate patient confidentiality, and are civil. Differing opinions are welcome as long as the tone is respectful.
Subscribe to:
Post Comments (Atom)





Once the patient crosses midnight into the new day, isn't he or his insurance charged for the whole day? Should he be rushed to go home if he prefers to take his time in getting ready to leave?
ReplyDeleteThanks, Anonymous.
DeleteYes, the 'day' for the purpose of payment begins at midnight. The blog has nothing to do with "rushing" people home. On the contrary, you may want to read the excerpt from a patient letter from the December 7, 2012 blog. Many of our patients get annoyed because they have to wait so long to leave after they are told that they can be discharged.
Once a patient is deemed stable enough for discharge home, why should it be OK for him/her to lounge around the room for another 10 to 12 hours? If we have 7 patients who have been discharged at 9 am and they decide they don't want to leave until they get two more meals, that's another nurse we have to bring in for patient care. And it's another patient who may be languishing in the ED wanting nothing more than to be in a comfortable bed. I've been a patient at another hospital in the area and believe me, when they tell you you're being discharged, they mean it!
ReplyDeleteThank you Dr. Chessare for committing to making this medical system the best place to work and to be a patient. I think the idea of changing the system of discharging a patient is a fantastic idea. My husband was a patient here on the medical floor a few years ago. He had been here for 5-6 days with a very bad pnuemonia and was very well cared for by the way! I remember coming to pick up my husband at 11:00, which is when I was told he'd be ready, and waiting until almost 4pm to take him home. I was very frustrated, because it seemed that all that needed to be done was for him was to get prescriptions, and for the nurse to do the actual discharge. Changing that system, will be wonderful for most patients and families I assure you. So now I am a nurse here, been for almost 6 months, and I am proud of it. I am also proud to work in a system that is working on itself.
ReplyDeleteI quite agree with you Dr.Chessare,I am a nurse and do get frustrated with having to give patient one reason or the other for not being discharged after he/she must have been informed for quite sometimes.so,truly we need a change in our system.
ReplyDelete